
New Yorkers Denied Access to Drugs
Jeffrey D. Klein
October 19, 2009
-
ISSUE:
- Health
HIV/AIDS NEW YORKERS
DENIED ACCESS TO DRUGS
Report Finds NYC Latinos Have Limited Access to
HIV/AIDS Medication
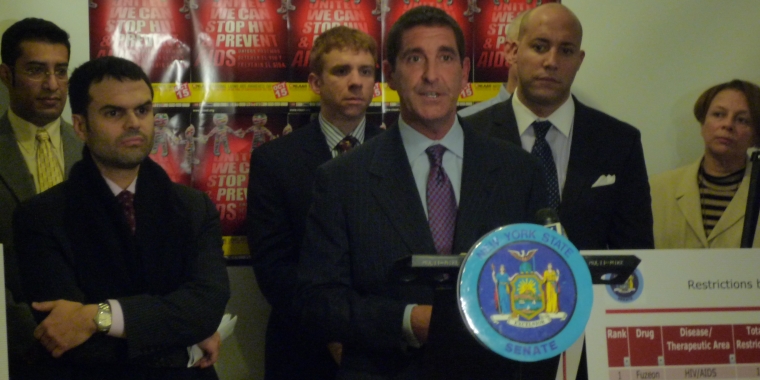
Empire State Pride Agenda, Latino Commission on AIDS, Pharmacists, Physicians and Elected Officials Rally for Life-Saving Drugs
NEW YORK- On “National Latino AIDS Awareness Day,” Senator Jeffrey D. Klein (D-Bronx/Westchester) joined by Empire State Pride Agenda’s Executive Director Alan Van Capelle, Latino Commission on AIDS’ Daniel Leyva, National Association of People With AIDS Director of Public Policy Matt Lesieur, Bronx Pharmacist Ray Macioci, representatives from the Gay Men’s Health Crisis and Dr. Antonio E. Urbina, MD with St. Vincent’s Comprehensive HIV Center rallied against NYS insurance companies who restrict access to brand name prescription drugs vital to HIV/AIDS treatment, for which there are no generic equivalents.
Klein released the results of an investigation into 12 major insurance providers in New York State detailing how they regularly and repeatedly roadblock coverage of what are known as “single-source drugs.” Single-source drugs are unique, patented brand name medications, for which there are no generic alternatives. If a drug is named a “single-source drug,” it means there is no other drug on the market that has the same chemical composition and arguably no other drug that has the same effectiveness.
The report documents tactics used by insurance companies to restrict coverage to patients from
accessing these vital drugs that are unique in their formulations but whose costs reduce insurance company profits.
“This is a matter of life and death. Access to single-source prescription drugs is particularly important in treating HIV/AIDS,” said Klein. “People with HIV/AIDS who desperately need these drugs for treatment are waiting too long as they battle the red tape strung out by insurance companies. We must put an end to these restrictions and get people the treatment they need immediately. ”
“It is absolutely reprehensible that people living with HIV/AIDS should have to worry about whether or not their insurance will cover their prescriptions,” said Alan Van Capelle, Executive Director of the Empire State Pride Agenda. “These medicines literally mean life and death for thousands of New Yorkers. Senator Klein’s bill will do away with this shameful practice once and for all and will let doctors and patients—and not insurance companies—decide what’s best for treatment.”
“Getting the right treatment in time can be a lifesaving issue for people living with HIV disease. And for all of us it’s a quality of life issue. Each medication to fight HIV has its own particular effects, and different individuals respond in different ways - no two of us are exactly the same. Treatment decisions -- which drugs to take and when -- should be made by patients and our doctors, working together for the health of the patient, not by insurers working for a healthier profit margin,” said John Hatchett, a NYC resident living with HIV.
“It is inconceivable that in New York State people living with HIV would be cut off from the drugs and treatment, as prescribed by their doctor, that they need to remain alive and healthy. Insurance companies should not be allowed to gamble with people’s lives in order to save a few dollars. This report highlights the need for Albany to enact legislation and regulations that require insurance companies to automatically fully cover all FDA-approved HIV medications, without any stop-loss provisions, prior authorization, exclusions from drug formularies, ridiculously low dispensing limitations or extremely high co-pays. There should be no barriers to accessing these life saving medications," said Matthew Lesieur with the National Association of People With AIDS and Village Care of New York.
According to the NYC Department of Health, as of 2007 nearly 120,000 individuals in New York City are currently living with HIV or AIDS. African Americans and Latinos are the highest populations living in NYC with HIV/AIDS at 46,283 (or 45%) and 32,630 (31%) respectively.
Manhattan has the highest percentage of individuals living with HIV/AIDS at 30.3%, Brooklyn falls close behind with 24.6% and the Bronx ranks third at 21.7%.
The Bronx is home to the highest number of Latinos living with HIV/AIDS in NYC with 6,745 or 29.5% Latino males and 4,051 or 41.6% of Latinas. Manhattan has the second highest number of Latino males living with HIV/AIDS at 6,568 or 28.7%. Brooklyn has the second highest number of Latino females living with HIV/AIDS at 2,138 or 22%.
“The insurance companies are endangering the lives and health of NYS’s HIV positive population, the largest in the nation, by restricting and denying their access to life saving HIV medications,” said Antonio E. Urbina, MD with St. Vincent’s Comprehensive HIV Center. “Insurance companies deny patients’ access to these drugs by denying to cover the HIV medications, capping the number of times prescriptions can be filled or by charging co-pays that are too expensive for patients to afford. The lack of access to the most effective therapies leads patients to miss doses, quit their therapies or drop out of care altogether. Further, these actions will endanger the health of all New Yorkers as HIV positive persons on suboptimal therapy have higher levels of virus circulating in their blood and genital secretions and are thus more likely to transmit the virus to others.”
Reports from the Centers for Disease Control and Prevention (CDC) show that Latinos are almost three times as likely to die of AIDS, and are more likely than members of any other race/ethnicity (41%) to receive an AIDS diagnosis less than 12 months after first being diagnosed with HIV.
“Latinos already make up the largest uninsured population in the nation, and it is reprehensible that even those of us who are fortunate enough to have insurance coverage might still be denied access to life saving medications because insurance companies want to save money,” stated Daniel Leyva, Director of HIV Prevention Services. “The Latino Commission on AIDS applauds Senator Klein for unveiling the behavior of major HMO’s and we look forward to supporting his legislation that would require insurance companies to cover these much needed drugs for our community.”
Klein’s investigation found that 12 major NYS health insurance companies regularly restrict access to approximately 15 different prescription drugs used in the treatment of HIV/AIDS. Further, the report showed how the majority of companies surveyed restrict access to HIV/AIDS related drugs anywhere from approximately 30-100% of the time. The investigation also found that the top five most common HIV/AIDS drugs had anywhere from four to eleven restrictions put on gaining access to them from the majority of NYS health insurance companies.
The following twelve NYS health insurance companies were surveyed in Klein’s report:
Aetna Health, Inc., Capital District Physicians’ Health Plan, CIGNA Healthcare of New York, Connecticare of New York, Empire HealthChoice HMO (incl. Empire BCBS HMO), Excellus Health Plan, GHI, Health Insurance Plan of Greater NY, Health Net of New York, Health Now New York, Independent Health Association, MVP Health Plan.
“This important legislation introduced by Senator Klein and Assemblyman Espaillat will have a positive impact for all patients being treated with brand-name prescription drugs for a wide variety of medical conditions. Most HIV/AIDS drugs are brand name (not generic), and by and large are extremely expensive,” said Ray Macioci with the Pilgrim Pharmacy and NYC Pharmacists Society. “This legislation would set co-payment limits and establish a cap on the patients' out-of -pocket expenses for pharmacy benefits, thereby enabling these patients to have uninterrupted therapy, a crucial aspect in the treatment of HIV/AIDS.”
Klein’s investigation showed that NYS insurance companies primarily restrict access by requesting that the physician prescribe alternative drugs, which experts say are often not the safest or most effective treatment for the patient. The average brand name drug is three times the price of the average generic drug ($119.51 vs. $34.34). HIV/AIDS brand name drugs typically cost much more, ranging from hundreds of dollars to more than $2,000 dollars per month.
In addition to expensive co-payments, insurance companies used the following so-called “cost containment strategies” to prevent patients from accessing drugs their doctors prescribed: 1) Prior Authorization from a doctor - which requires time-consuming phone calls and paperwork for doctors and patients alike and can involve appeals that take days or weeks to resolve, 2) Quantity Limitations -which limits the amount of medication or number of prescriptions that can be purchased at one time, 3) Exclusion- excludes expensive medications from the formulary altogether, therefore the drug is not covered for the insured, and 4) Mandatory Mail Order- insurer only provides coverage for the drug when it is purchased through the insurer’s designated mail-order pharmacy.
Among the significant findings in Klein’s report:
• Excellus restricted the most drugs surveyed, with restrictions on 100% of the total drugs investigated. Aetna restricted the second highest number drugs with restrictions on 40% of the total drugs investigated. (See page 22 in report). Aetna also had the highest co-pay for six HIV/AIDS drugs (See page 21).
• Fuzeon was the most restricted HIV/AIDS drug with 11 total restrictions placed on the drug by 7 different HMOs.
• Atripla was the second most restricted HIV/AIDS drug with 6 total restrictions placed on the drug by 6 different HMOs.
Klein urged fellow lawmakers to pass Klein’s proposed bill (S2938) and the Assembly bill (A8863) sponsored by Espaillat, which take a variety of measures to reduce limitations on access to brand-name patented drugs.
“GMHC fully supports the efforts of Senator Klein to ensure the best possible prescription plans are made accessible to New Yorkers living with HIV/AIDS. Physicians should be able to prescribe what they deem as the most effective course of treatment to a patient regardless of drug costs or insurance coverage,” said Sean Cahill, Ph.D. Managing Director of Public Policy for Research and Community Health with Gay Men’s Health Crisis.
# # #
Share this Article or Press Release
Newsroom
Go to NewsroomSenator Klein Celebrates Black History Month
February 18, 2006

Senator Klein Announces Return Of Crossing Guard To P.s. 71 Intersection
February 15, 2006

Klein Slams Bloomberg Decision To Shutter Woodlawn Firehouse
February 10, 2006
