
Sen. Farley Says Tougher Medicaid Fraud Effort Needed
Hugh T. Farley
March 8, 2010
-
ISSUE:
- Medicaid

State Senator Hugh T. Farley (R, C, I - Schenectady) and his fellow members of the Senate Republican Task Force on Medicaid Fraud conducted a public forum today in Albany to investigate what savings can be gained from New York’s overburdened Medicaid system. The task force will explore ways in which the State Legislature can assist counties to improve Medicaid fraud prevention efforts, as well as develop recommendations for improving the State’ Medicaid system.
Among those providing expert testimony today were Nassau County District Attorney Kathleen Rice, New York State Association of Counties President Thomas J. Santulli, District Attorney’ Association of New York President Kathleen Hogan, Rensselaer County Executive Kathleen Jimino, Albany County Comptroller Mike Conners and Medicaid fraud technology specialists.
Along with Senator Farley, the task force includes Senators George Winner (R-C-I, Elmira), Charles Fuschillo (R, Merrick), Michael Nozzolio (R-C, Fayette), Mike Ranzenhofer (R-C-I, Amherst), Martin Golden (R-C, Brooklyn) and Vincent Leibell (R-C-I, Patterson). The task force is chaired by Senator Kemp Hannon (R-C-I, Garden City).
Despite the fact that they are on the front lines of the Medicaid program, county officials are saying the State hinders their efforts to stop fraud at the local level. In fact, the 2009-10 State Budget approved by the Governor and Democratic legislators eliminated the eligibility requirements for county-conducted face-to-face interviews, finger-imaging and asset tests for Medicaid applicants, conducted by counties. The interviews are intended to ensure accountability in the system, but will no longer be required as of April.
The Executive Budget proposes spending a total of $52.5 billion on Medicaid, meaning as much as $5 billion could be fraud in the system.
In December, the New York State Comptroller released the results of an audit that identified as much as $92 million in Medicaid overpayments, billing errors and other problems. He called on the State Department of Health to increase scrutiny of Medicaid payments and recover payments that were improperly made. The Department agreed there were overpayments, but said it would only try to recover $2.4 million in overpayments.
In addition, a 2008 report in the New York Post cited an audit by the Comptroller’s Office, determining that nearly 30,000 people in New York City alone were improperly enrolled in the State’s Medicaid system between November 2006 and November 2007. The audit shows that almost 13,000 former New York City residents should have been investigated for violations of the State’ Medicaid laws, only 207 cases were investigated.
In his Executive Budget, Governor Paterson increased the State’s target for Medicaid fraud recovery by $300 million, to a total of $1.1 billion.
Share this Article or Press Release
Newsroom
Go to NewsroomSenator Farley Highlights Buddy Walk
September 28, 2015
Senator Farley Enjoys Indian Lake's Moose Festival
September 28, 2015

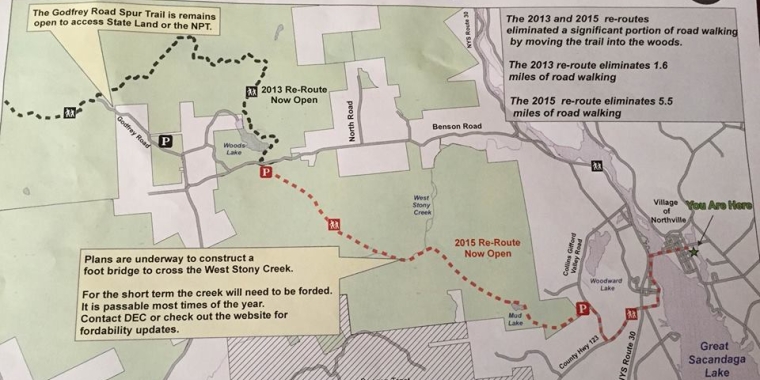
23-Mile Northville-Placid Trail Rerouting Now Complete
September 24, 2015
Sept. 20th - 26th is National Farm Safety and Health Week
September 23, 2015
